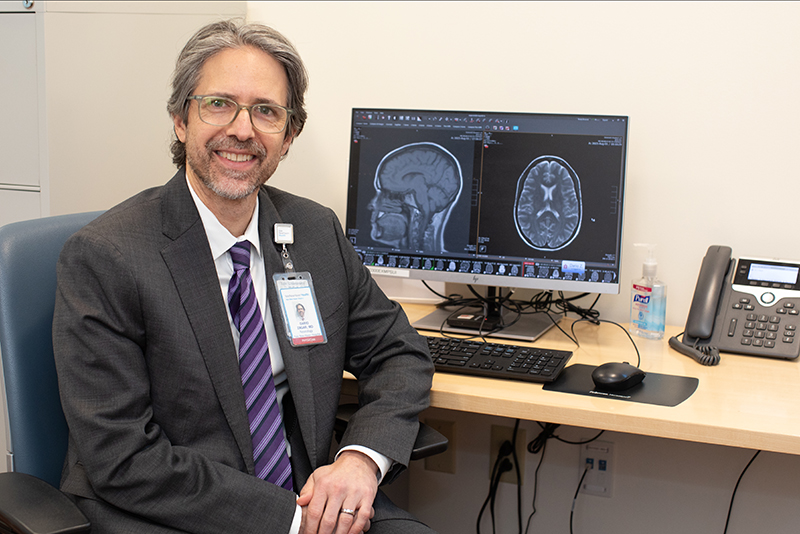
A migraine can be a big headache but knowing your treatment options can help. Learn more about migraine in this Q&A with Dario Zagar, MD, a neurologist affiliated with Bridgeport Hospital and Yale New Haven Hospital.
Is it a headache or a migraine? If you’ve ever had a migraine, you are painfully aware of the difference.
Nearly 40 million Americans get them, a statistic that means someone is living with migraines in one out of every four households in the United States. Dario Zagar, MD, a neurologist affiliated with Bridgeport and Yale New Haven hospitals, is associate professor of Neurology at Yale School of Medicine. He sat down with Healthy & Wise to explain how a migraine differs from a headache in this Q&A.
Who is most likely to get migraines? Are there specific risk factors that make people predisposed to getting them?
Migraine often runs in families, suggesting that there is a significant hereditary component. Women are about three times as likely as men to have migraine. The incidence of migraine is also higher in younger people between the ages of 18 - 44.
What differentiates a migraine from a headache? What are the symptoms?
As someone who has suffered from migraines myself, I can attest to the fact that migraine is much more than “just a headache.” The hallmark of migraine is a moderate to severe headache, which may be throbbing and on one side of the head, though not always, and it feels better with rest. However, it is the associated symptoms, such as nausea and vomiting, sensitivity to light and sound, and dizziness that can be truly disabling for some people. Some migraine sufferers can have symptoms that come before the headache. These symptoms, referred to as an “aura,” most commonly consist of visual distortions like shimmering lights, zigzag lines or loss of vision.
Are there triggers for migraines? How can I figure out what my triggers may be?
The most commonly reported migraine triggers are stress and hormonal changes. People with migraine are more sensitive to changes in routine and environment, so other common triggers include alterations in sleep (not getting enough sleep or even getting too much), inadequate hydration and nutrition, weather changes and alcohol. Some foods can be a trigger. We typically recommend that new patients keep a headache diary, perhaps with an app like Migraine Buddy or N1-Headache™, to assess their headache frequency and to look for possible triggers.
What are some treatments for migraine?
First off, it is important to have an effective abortive treatment, which is something to be used at the onset of a migraine to make it go away more quickly. Over-the-counter medications are often used as first-line treatment for migraine. These include non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil®, Motrin®), naproxen (Aleve®) and aspirin; and acetaminophen (Tylenol®).
The most commonly used prescription abortive medications are the triptans, such as sumatriptan (Imitrex®) and rizatriptan (Maxalt®). There is a newer class of agents called gepants, including rimegepant (Nurtec®) and ubrogepant (Ubrelvy®), that may be beneficial if triptans are not effective or appropriate. For a migraine that just won’t go away, we may have patients come to our infusion center for intravenous treatment.
People with more frequent migraines may also need a preventive strategy. I’m particularly interested in nonmedication approaches. These include vitamins and herbal supplements, diet and exercise, acupuncture and mind-body treatments. We are learning more about how stress and trauma may impact painful conditions including migraine, and addressing those issues can be important.
For some people, prescription medications may be appropriate. Many of the preventive medications were initially intended to treat other conditions, like depression, seizures and hypertension, and later found to be helpful to prevent migraines. In recent years, we finally have treatments that were specifically designed to prevent migraines, called calcitonin gene-related peptide – or CGRP – inhibitors that have revolutionized the field. These can be given orally, like the gepants, by monthly injection or every three months intravenously. For very frequent migraines, Botox® injections are also an option.
When should I seek medical attention and/or talk to a doctor?
If your migraines are frequent or are disrupting your life, it is worth speaking to a physician. Unfortunately, most people with migraines never seek medical care for their condition, and many don’t even know that they have migraines! Now is a very exciting time in headache medicine, and it is worthwhile getting treatment from a specialist. Even if you don’t like the idea of taking medication, there are other options that can make a huge difference.
Seek immediate medical attention if your headaches have appeared suddenly or if you experience symptoms like weakness, fever, confusion or any neurological deficits. These can be a sign of a more serious condition.
Bridgeport Hospital specialists use innovative technologies and techniques to diagnose and treat patients with a host of neurological conditions, including migraines and headaches.